UNIVERSITY PARK, Pa. -- Compounds that stop a cellular rescue operation for stuck ribosomes may bolster the nation's defenses against biowarfare and bioterrorism, as well as create alternative antibiotics to handle increasingly resistant pathogens, according to a team of researchers.
In a study of macrophages -- white blood cells -- from animals, researchers used two inhibitors -- KKL-10 and KKL-40 -- to stop the proliferation of Franscisella tularensis, bacteria that the U.S. Centers for Disease Control classifies as a tier 1 select agent because the strain is highly infective and easily spread, said Kenneth Keiler, professor of biochemistry and molecular biology, Penn State.
The compounds target ribosomes in the translation phase of the bacteria's genetic process, he added. For bacteria to grow and proliferate, protein-generating ribosomes, like engines rolling down a track, must travel down the messenger RNA (mRNA) to translate additional proteins. However, when the ribosomes become stuck, the bacteria dispatches ribosome rescue factors -- tmRNA, ArfA and ArfB -- to free the ribosome.
Keiler said that KKL-10 and KKL-40 were able to halt this rescue operation in the bacteria without damaging host cells.
"At the beginning of the study, we identified compounds that block rescue of ribosomes that are stuck on mRNA, and these have antibiotic activity against a number of pathogens that we can test in the lab," said Keiler. "In this study, first, we wanted to test the compounds against a pathogen that is important for biodefense and we also wanted to make sure that these compounds would work inside eukaryotic cells."
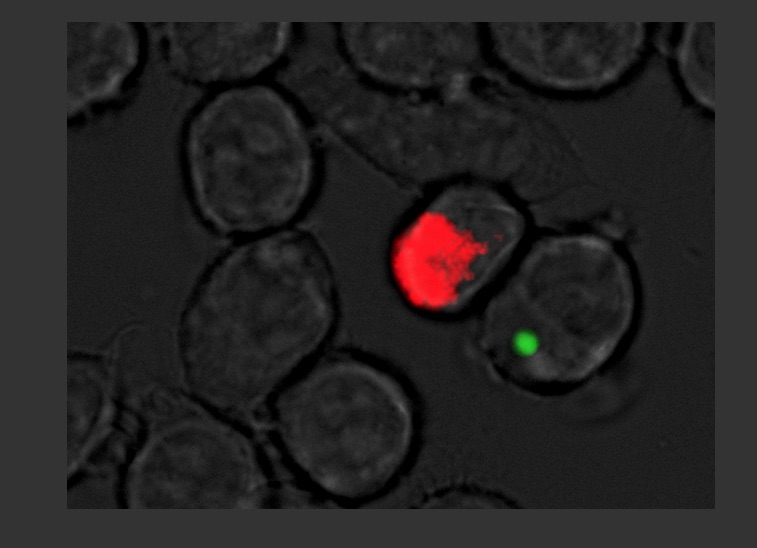
Figure. Penn State researchers developed antibiotic compounds that stopped Franscisella Tularensis, a virulent strain bacteria used in biowarfare, from spreading in animal cells.
Franscisella tularensis can cause fatalities in up to 60 percent of the cases if left untreated, said Girish Kirimanjeswara, assistant professor, veterinary and biomedical sciences, Penn State, who worked with Keiler. It was also stockpiled as a biowarfare agent during the Cold War.
"In today's world of terrorism, it is essential that we are well-prepared to defend ourselves and our military personnel against biowarfare agents," said Kirimanjeswara. "In that regard, finding new targets and antibiotics against these agents is critical and our research shows that these compounds may be very attractive way to treat bacterial diseases."
After decades of using antibiotics to kill pathogens, more and more diseases have become resistant to conventional drugs and treatments, according to the researchers, who report their findings in Antimicrobial Agents and Chemotherapy, currently available online. This has increased the urgency to find new drugs and new ways of stopping pathogens.
"There are many pathogens that are resistant to all existing antibiotics -- if you are infected with one of these totally resistant strains and show up in the clinic there's nothing the doctors can do for you," said Keiler. "If your immune system can fight off the infection, you'll survive and if it can't, you die. It's back to pre-1940s-era medicine. If we don't develop new drugs and the resistant genes are going to continue to spread, more and more diseases will become untreatable."
He suggests that because the researchers are using a new compound and targeting a new pathway, Franscisella tularensis -- and possibly other pathogens -- may struggle to adapt resistance to the treatment.
"One of the good things about our compounds is this is a new chemical, so it's unrelated to any of the existing drugs, which means maybe there may not be enzymes out there to modify those drugs and inactivate them," said Keiler. "Although we won't know that until we get into the clinic."
Kirimanjeswara said that Franscisella tularensis is difficult to stop because it can survive both outside and inside the cell, as well as in different compartments of host cells.
"This strategy allows bacteria to survive and escape from host immune responses, for example, within the host cells, and there are not many antibiotics that can target a bacterium in all these compartments," said Kirimanjeswara. "In that regard, these compounds were effective outside the cells, in the various stages of endocytic vesicles, and in the cytoplasm, making it a very attractive way to treat bacterial diseases."
The next steps for the research will be to experiment on delivery designs and to test the compounds in animals.
The researchers carried out the study at Penn State's Eva J. Pell Laboratory for Advanced Biological Studies. Research in the laboratory is centered on global food and health security with special emphasis on diagnosis, prevention and therapeutics against highly infectious diseases.
Keiler and Kirimanjeswara also worked with Tyler D. P. Goralski and Kalyan K. Dewan, graduate students, biochemical and molecular biology; John N. Alumasa, postdoctoral scholar, biochemical and molecular biology; Victoria Avanzato, former undergraduate student, immunology and infectious disease; David E. Place, former graduate student, veterinary and biomedical sciences; Rachel L. Markley, graduate student, immunology and infectious disease, and Bhuvana Katkere, postdoctoral scholar, veterinary and biomedical sciences, all of Penn State, and Seham M. Rabadi, graduate student, and Chandra Shekhar Bakshi, assistant professor of microbiology and immunology, both of the New York Medical College.
The National Institutes of Health and The Huck Institutes of the Life Sciences supported this work.
Story by Mat Swayne
Written By: Goralski TD, Dewan KK, Alumasa JN, Avanzato V, Place DE, Markley RL, Katkere B, Rabadi SM, Bakashi CS, Keiler KC Kirimajeswara G
Paper Url: http://aac.asm.org/content/early/2016/03/02/AAC.03089-15.long
Paper Id: 10.1128/AAC.03089-15
