Although Plasmodium falciparum is the most deadly species of human malaria, disease caused by another species, P. vivax, threatens the health of a greater number of people globally, in part because vivax malaria has the alarming ability to reappear in the bloodstream of an individual months, or even years, after the person is “cured.”
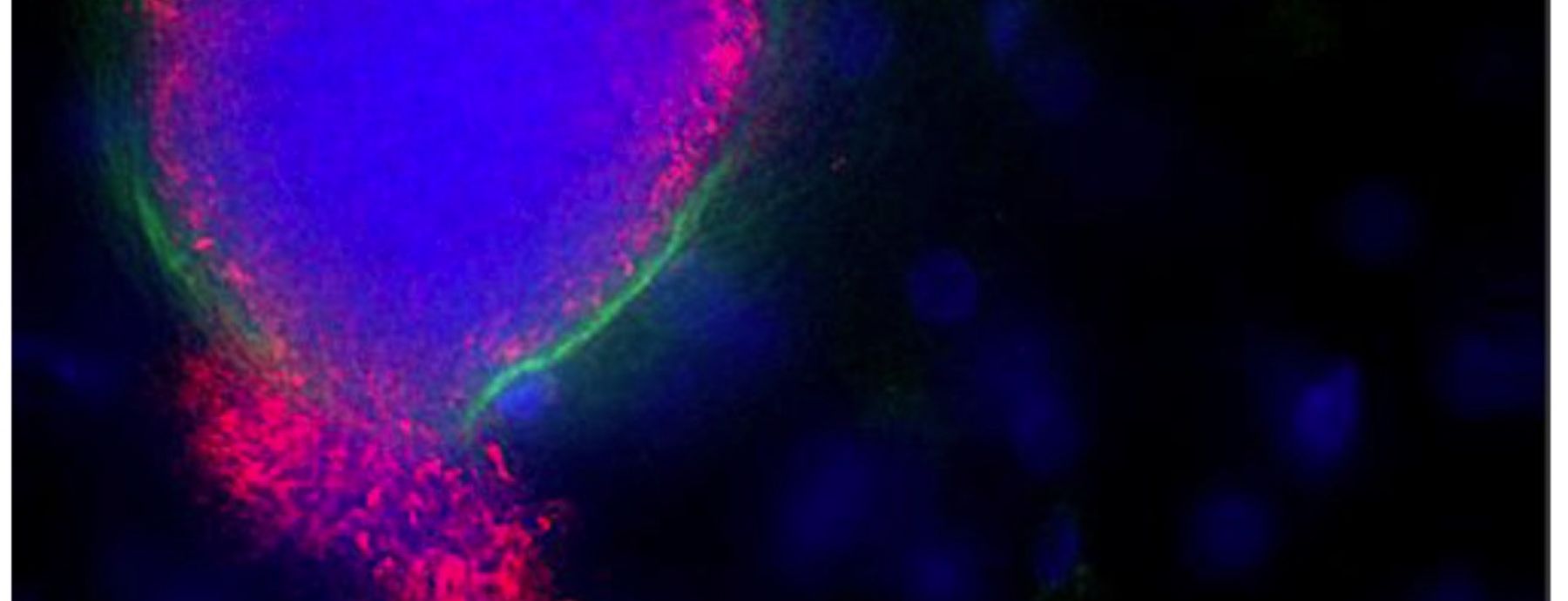
P. vivax infections relapse when a fraction of parasites, rather than bursting out of the liver into the bloodstream to initiate the symptoms of an acute infection, develop into dormant liver stages called hypnozoites. Studying hypnozoites is difficult, complicated by the fact that P. vivax infects the cells of humans or non-human primates, and that rodent-infectious species do not produce hypnozoites. To address this problem, a team of researchers from Mahidol University in Thailand, Seattle Biomedical Research Institute, University of Washington and Penn State, including CIDD researcher Scott Lindner, developed an in vitro model system using mice transplanted with human liver cells.
In the newly developed system, P. vivax completes liver-stage development and generates persistent hypnozoites, which will allow for studies of the liver-to-blood-stage transition, as well as studies of hypnozoite response to drug treatment in humanized mouse hosts. The potential contribution of their system to drug studies is of particular interest, as only one drug is currently approved to prevent or eliminate vivax malaria infections in humans.
The research was published in Host Cell & Microbe and can be found here.
Synopsis written by Katey Glunt and Jo Ohm.
Written By: Mikolajczak SA, Vaughan A, Kangwanrangsan N, Roobsoong W, Fishbaugher M, Yimamnuaychok N, RezakhaniN, Lakshmanan V, Singh N, Kaushansky A, Camargo N, Baldwin M, Lindner SE, Adams JH, Prachumsri J, & Kappe SHI
Paper Url: http://www.cell.com/cell-host-microbe/abstract/S1931-3128%2815%2900068-2
Paper Id: http://dx.doi.org/10.1016/j.chom.2015.02.011